If You Notice Cracks at the Corners of Your Mouth, Here’s What Your Body Is Signaling…
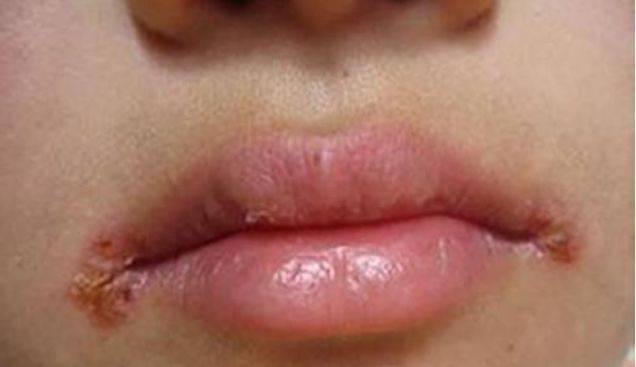
You’re going about your day—smiling at a grandchild’s joke, taking a bite of an apple, or simply yawning—when a sudden, sharp sting at the corner of your mouth stops you cold. Ouch. You touch the spot and feel it: a small, angry crack or split in the skin. It might be red, flaky, or even oozing a little. You’ve got what’s often called “angular cheilitis,” but you probably know it as just those annoying, painful splits at the corners of your lips.
Your first thought might be, “Is this just chapped lips?” But while lip balm might offer temporary relief, it rarely fixes the problem if it keeps coming back. That’s because these cracks aren’t usually about the lips themselves. They’re more like a tiny, flashing neon sign from your body, pointing to something happening inside.
Think of the corners of your mouth as a vulnerable crossroads. It’s where the sensitive skin of the face meets the even more delicate mucous membrane of the lips. It’s a warm, moist fold—perfect for saliva to pool, especially if you sleep with your mouth open or have deep laugh lines. But that moisture is a double-edged sword. It can lead to a perfect storm of factors, and your body uses this specific location to send up a flare.
So, what exactly is that flare signaling? Let’s decode the messages.
Message #1: “We’re Running Low on Key Supplies.” (The Nutritional Deficiencies)
This is one of the most common signals for recurring angular cheilitis. Your body is telling you it’s deficient in specific vitamins and minerals crucial for skin health and immune function.
- The B-Vitamin Brigade (Especially Riboflavin – B2, and B12): B vitamins are essential for maintaining healthy skin and mucous membranes. A deficiency can cause them to become fragile and easily cracked. This is especially notable in B12 deficiency, which can also cause a sore, red tongue. Older adults, those on restrictive diets (like vegan diets without proper supplementation), and people with conditions affecting absorption (like celiac disease or Crohn’s) are at higher risk.
- The Iron Connection: Iron deficiency anemia doesn’t just make you tired. It can lead to poor oxygen delivery to tissues, weakening them and making them more susceptible to breakdown and infection. Angular cheilitis is a classic, though often overlooked, sign of low iron.
- Zinc: This mighty mineral is vital for wound healing and immune response. Without enough of it, small cracks like these don’t get the signal to repair themselves properly.
Message #2: “There’s a Microbial Party, and It’s Getting Out of Hand.” (The Infection Angle)
Remember that warm, moist environment? It’s a prime rental space for microorganisms.
- Yeast (Candida): This is a frequent culprit. The constant moisture creates a fungal paradise. Candida, which normally lives harmlessly in our mouths, can overgrow and infect the broken skin, leading to persistent, itchy, often whitish cracks that don’t heal with simple lip balm.
- Bacteria (Staph or Strep): Sometimes bacteria seize the opportunity, especially if the initial crack was from dryness or irritation. This can lead to more inflamed, crusty, or pustular sores.
Often, it’s a combination: a nutritional deficiency weakens the skin barrier, saliva irritation breaks it down, and then an infection (fungal or bacterial) moves in and sets up camp, preventing healing.
Message #3: “The Local Environment is Too Harsh.” (The Mechanical & Local Factors)
Sometimes the signal is about a very local issue.
- The Pool of Saliva: This is a huge factor. If you have ill-fitting dentures that don’t support the face properly, allowing the corners of the mouth to sag and pool saliva, you’re creating the problem. Sleep apnea, leading to mouth breathing, or simply the natural loss of collagen and elasticity with age (which deepens those folds) can have the same effect.
- The Lick Cycle: It’s an instinct: something feels dry and irritated, so you lick it. Saliva contains digestive enzymes designed to break down food. On delicate skin, these enzymes end up breaking down the skin itself, leading to more dryness, more cracking, and more licking—a vicious, painful cycle.
- Allergies & Irritants: Certain ingredients in toothpaste (like sodium lauryl sulfate), mouthwash, or even lip products can cause a contact dermatitis that manifests at the corners. Flavored or acidic foods (citrus, tomatoes) can also be irritants.
Message #4: “Check the Bigger Picture.” (The Systemic Health Link)
Persistent angular cheilitis that doesn’t respond to simple treatments can occasionally point to broader health conditions.
- Diabetes: High blood sugar creates an environment where yeast (Candida) thrives. Unexplained or frequent fungal infections, including at the mouth corners, can be an early clue to undiagnosed or poorly controlled diabetes.
- Autoimmune Conditions: Conditions like Sjögren’s syndrome, which severely dry out mucous membranes (eyes and mouth), can lead to chronic angular cheilitis due to the constant dryness and fragility of the tissues.
- Immune Suppression: Any condition or medication that weakens the immune system can allow normally harmless microorganisms to become problematic.
What to Do When You See the Signal: A Practical Action Plan
Ignoring these cracks is like ignoring a “Check Engine” light. Here’s how to respond:
- Start with Meticulous, Dry Gentle Care: Break the moisture cycle. After eating or drinking, gently pat the corners of your mouth dry. Use a thick, plain emollient like petroleum jelly or a zinc oxide cream (like a diaper rash ointment) as a barrier. Apply it before bed and before meals to protect the area. Crucially, stop licking!
- Review Your Diet & Consider a Supplement: Take an honest look at your nutrition. Are you eating a varied diet rich in leafy greens, lean proteins, whole grains, and nuts? If you’re on a restrictive diet, consider a high-quality multivitamin or a B-complex supplement. However, don’t just start megadosing—aim to get nutrients from food first.
- Check Your Dental Hardware: If you wear dentures, see your dentist. Ill-fitting dentures are a prime cause. They may need adjustment or relining. Also, practice excellent denture hygiene, including nightly cleaning and soaking in an antifungal solution if recommended by your dentist, as dentures can harbor Candida.
- See Your Doctor or Dermatologist (This is Key): If the cracks persist for more than a week or two with simple care, it’s time for professional help.
- They can often diagnose by sight but might do a gentle swab to check for Candida or bacterial infection. This dictates the treatment.
- They may prescribe a topical antifungal cream (like nystatin or clotrimazole), an antibacterial ointment, or a combination cream with a mild steroid to reduce inflammation.
- They can order a simple blood test to check your levels of iron, ferritin (iron stores), B12, and other B vitamins. Addressing a deficiency is the only way to stop the problem from recurring if that’s the root cause.
- They can help investigate other underlying causes if suspected.
Those small cracks are more than a minor nuisance. They’re a form of communication from a body that’s remarkably good at showing us where imbalances lie. By listening to that signal—by looking beyond the lip balm aisle and into your nutrition, habits, and overall health—you can do more than heal a sore spot. You can address a small imbalance before it becomes a bigger one, and return to laughing, yawning, and enjoying that apple completely pain-free. After all, your smile deserves a comfortable home.
